You are working on a 15-page essay at 2 in the morning, and just as you start your concluding paragraph, a burst of pain shoots to your head. The pain lingers for another 4 hours before you call it quits and decide to write the rest of your essay after a good night’s (or morning’s?) rest. You attribute your migraine to your constant screen time and dehydration. What you may not realize is that there are many more factors that may be involved in this phenomenon.
On November 12th, Amherst College had the privilege of hosting Pamela Rist, ScD, an Assistant Professor at Harvard Medical School and at Harvard T.H. Chan School of Public Health. She also is an Associate Epidemiologist in the Division of Preventive Medicine at Brigham and Women’s Hospital. She discussed the migraine as well as its risk factors and future research directions upon understanding this phenomenon.
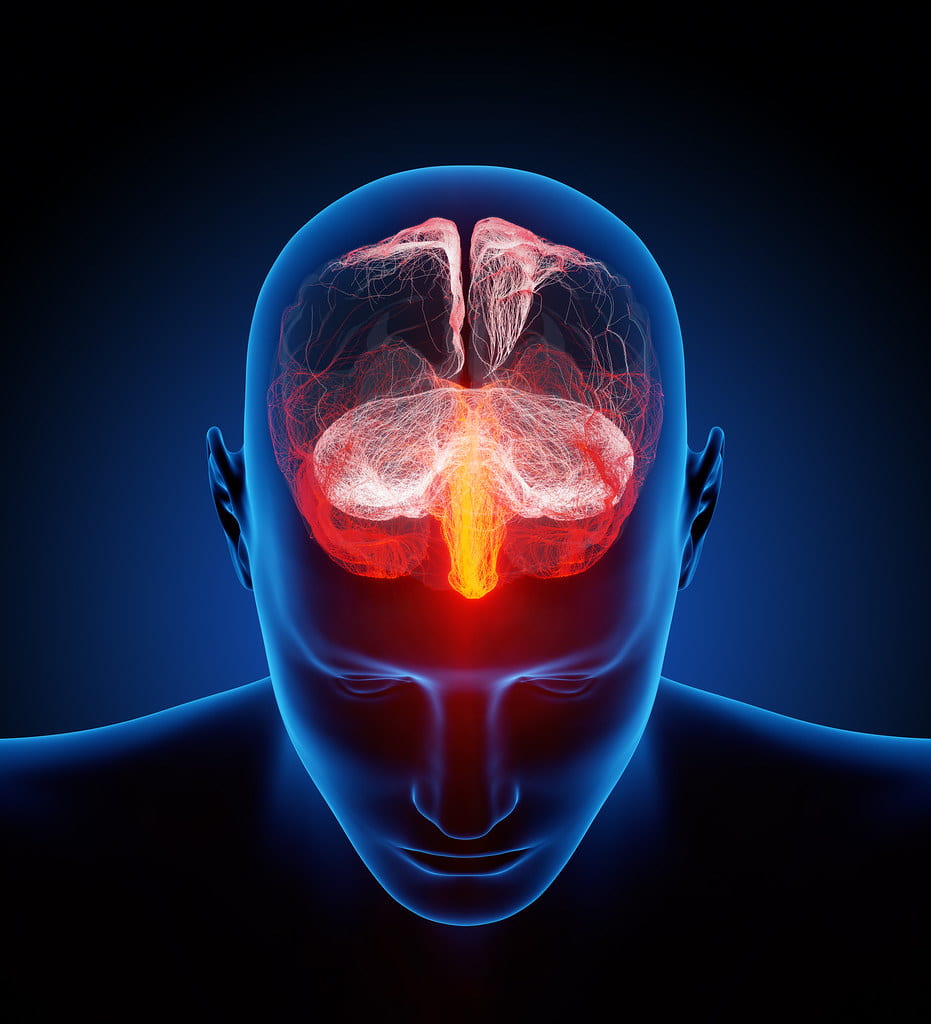
According to Professor Rist, a migraine is a “chronic intermittent primary headache disorder that involves the neuronal system.” It can range in severity, from moderate to pulsating, depending on the situation and the individual. Even though it can range in severity there are certain “requirements” that must be met in order to diagnose a migraine. It usually lasts approximately 4-72 hours, and must have two of the following characteristics: unilateral location, pulsating quality, moderate or severe pain intensity, and aggravation by routine physical activity. The migraine can also be associated with “aura,” which is a recurrent disorder that results in reversible focal neurological symptoms.
Professor Rist then discussed the migraine’s significance in a national perspective. Approximately 15% of the US population experiences migraines, with women afflicted twice as often as men. Migraines are usually most intense in people in their 30s.
Migraines and their associations with cardiovascular disease is not a new one: it has been described and examined for many years. Migraines roughly double the risk of ischemic stroke, and have been associated with heart attacks and angina. As a result of many other risk factors, it is too difficult to produce a perfectly accurate relationship between migraines and their effect on cardiovascular phenomena. To examine migraine and cardiovascular disease (CVD) risk factors, Professor Rist mentions her “Women’s Health Study.” This is a study that started in the 1990s with randomized, placebo-controlled trials of the effects of low-dose aspirin and vitamin E in the primary prevention of CVD and cancer. It has continued as more of an “observational follow-up” of the 39,876 women involved at the start of the study. This “observational follow-up” involved a questionnaire that asked the participants whether or not they have ever had a migraine. The main takeaway from this study was that women with migraine with aura had a higher incidence rate of self-reported major CVD events as compared with women without migraine or with migraine without aura, with the adjustment of other confounding risk factors that may have been involved.
Migraines and their association with cognitive decline has also proved to be important as well. Migraine has been linked to an increased risk of vascular events and silent brain lesions, for example, and has been labeled by some as a “progressive brain disorder.” The Women’s Health Study tackled this question by assessing cognitive function of women 65 years of age and older (who experienced migraines) through verbal memory exercises and language and executive functioning exercises. Through these assessments, they discovered that there is no evidence that migraine is associated with greater rates of cognitive decline.
Some methodological challenges associated with migraine include the phenomenon of migraines “resolving” (i.e. no longer experience the headache pain) as individuals age and the unknown of how changes in migraine frequency and characteristics over time influence cardiovascular disease risk.
Professor Rist concluded her talk with future directions about this topic. These include repeated assessments of migraine status over time and the role of migraine medications in disease risk and long-term outcomes. She confirms that there is still much to learn before we know the answers.
While the migraine has been overlooked by many, we can all take steps in learning more about this phenomenon and how much it has affected other physical phenomena. I want to thank Professor Rist for providing an excellent talk and for her contributions in providing this picture for us to view.